Friday, April 17, 2015
Saturday, April 11, 2015
Thursday, April 9, 2015
Increased Carbohydrate intake is far more important cause of obesity than increased Fat intake.
الدراسات السكانية وبيانات المسوح تظهر انخفاضا في نسبة السعرات الحرارية الغذائية من الدهون خلال التسعينيات 1990s ولكن زيادة في انتشار السمنة (Prentice and Jebb, 1995 and www.cdc.gov/nchs/nhanes.htm)
وكان هذا الانخفاض في نسبة من النظام الغذائي من السعرات الحرارية من الدهون على الرغم من الزيادة الإجمالية في استهلاك السعرات الحرارية وبالتالي فإن القيمة المطلقة من الدهون في النظام الغذائي ثابتة نسبيا. أيضا، انخفضت مستويات النشاط البدني خلال نفس الفترة والتي يمكن أيضا أن تسهم في زيادة نسبة البدانة. ومع ذلك، أثارت هذه البيانات، جنبا إلى جنب مع دراسات فقدان الوزن أن الوجبات الغذائية قليلة الدسم ليست أكثر فعالية لفقدان الوزن من الوجبات الغذائية الغنية بالدهون.
هذه الدراسات اظهرت اهمية المواد الغذائية الرئيسية الأخرى، تحديدا الكربوهيدرات بشكل رئيسي، في تطوير البدانة والتمثيل الغذائي الذي يؤدي إلى متلازمة الأيض بشكل خاص عن طريق تقليل الدهون في النظام الغذائي و بالتالى زيادة لاحقة في الكربوهيدرات الغذائية(CHO).
نوع الكربوهيدرات مهم ايضا على وجه الخصوص، لذلك فان نوعية الكربوهيدرات بدلا من كمية الكربوهيدرات في النظام الغذائي الان محور التحقيق المكثف.
Population Studies and data surveys show a drop in food calories from fat during the nineties 1990s, but an increase in the prevalence of obesity (Prentice and Jebb, 1995 and www.cdc.gov/nchs/nhanes.htm).
This decline was in the proportion of the diet of calories from fat in spite of the overall increase in calorie consumption and therefore the absolute value of fat in the diet was relatively constant. Also, levels of physical activity decreased during the same period, which can also contribute to increasing the proportion of obesity.
However, these data have raised, along with the weight loss that low-fat diets are not more effective for weight loss than high-fat diets studies.
These studies demonstrated the importance of other key nutrients, specifically carbohydrates mainly in the development of obesity and metabolic syndrome, in particular by reducing the fat in the diet and thus a subsequent increase in dietary carbohydrate (CHO).
Carbohydrate type is also particularly important, so the quality of carbohydrates instead of the amount of carbohydrates in the diet is now the focus of intense investigation.
http://www.weightforce.com/sliders/view/21
LIPID METABOLISM DURING EXERCISE
LIPID METABOLISM During EXERCISE
‘Fat burn’ really occurs in three major stages, these stages are shown in the diagram to the left.
During exercise, the body releases epinephrine and norepinephrine, (catecholamines).
Catecholamines act as a catalyst to the entire lipolytic pathway, and sets fat burn into motion by binding to the beta receptors (see the ‘β’ in the diagram) on the cell membrane.
Once these beta receptors are stimulated, ATP is converted to cAMP. This converted cAMP uses it’s phosphate group to bind and remove perilipins from the surface of the triglyceride, and hormone sensitive lipase (HSL) is allowed to cause the release of lipids (fat) into the blood stream.
(Sztalryd and colleagues et al 2003, Souza and colleagues et al 1998)
Figure 1 : Obesity: Be cool, lose weight : Nature
Figure 1 : Obesity: Be cool, lose weight : Nature

From the following article:
Stephen R. Farmer
Nature 458, 839-840(16 April 2009)
doi:10.1038/458839a

Adult humans seem to contain brown adipose tissue (BAT) primarily behind the muscles of the lower neck and collarbone, as well as along the spine of the chest and abdomen2, 3, 4. After food consumption, the absorbed fats and sugars are used to provide energy for daily functions, with excess calories being stored as fat in the white adipose tissue, which is mainly located under the skin of the buttocks and legs in women and around the internal organs in men. BAT can be activated in response to various stimuli, including exposure to cold, to burn fat and sugars. This process seems to be more prominent in the young and lean than in the old and obese, and in women rather than in men.
What is new in adipose tissue? - For Medical Professionals - Mayo Clinic
What is new in adipose tissue? - For Medical Professionals - Mayo Clinic
What is new in adipose tissue?
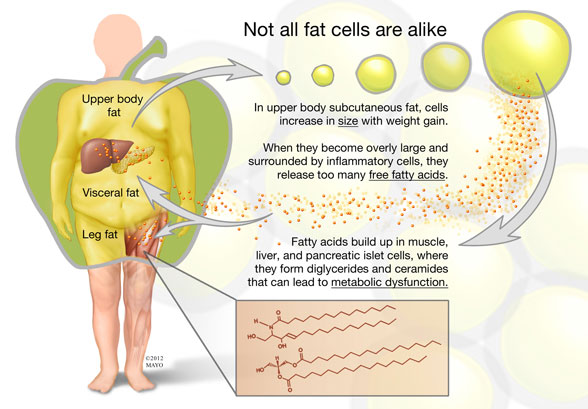
Men and women of normal weight have 15 percent and 30 percent body fat, respectively. Obese adults can have as much as 100 kg of body fat under extreme circumstances. The average size of a fat cell ranges from 0.2 to 1.4 mcg of lipid per cell, which means that someone with 20 kg of fat can have on the order of 33 billion fat cells. However, not all fat and not all fat cells are alike.
Michael D. Jensen, M.D., of the Division of Endocrinology, Diabetes, Metabolism, and Nutrition at Mayo Clinic in Rochester, Minn., says: "Our research program has focused largely on the attributes of human adipose tissue and body fat distribution as it relates to health and disease. For more than 20 years, we've been aware that persons with a preponderance of visceral (omental and mesenteric) fat and upper body fat are at greater risk for the metabolic complications of obesity. Persons with this body fat distribution also have greater concentrations of free fatty acid (FFA) in the blood."
Dr. Jensen continues: "It has been repeatedly shown that artificially elevating the FFA levels in healthy individuals can create insulin resistance and some of the other metabolic abnormalities seen in upper body obesity. One possible explanation is that those persons with excess visceral fat also take up and release too many fatty acids from the visceral fat. The adipocytes in the visceral fat, when studied in vitro, appear to have this potential. Excess FFA release from visceral fat could disproportionately affect hepatic metabolic function because the venous drainage of omental and mesenteric fat is into the portal vein — the so-called portal hypothesis.
"In contrast, adults with larger amounts of lower body (leg) fat often have relatively little visceral fat and have normal FFA levels. Our research has indicated that fat cells in visceral fat, leg fat and upper body subcutaneous fat have unique characteristics that make them almost completely different types of fat. We also have discovered that much of what was believed about the visceral fat in the portal hypothesis was not entirely correct."
Dr. Jensen explains: "For example, men and women with small visceral fat adipocytes have a much greater tendency to store fat in their visceral depot, probably because the levels of proteins and enzymes related to fat storage are quite high in these fat cells. However, as omental and mesenteric fat cells (and thus visceral fat mass) become larger, most of the proteins and enzymes related to fat storage are dramatically suppressed and the cells become resistant to fat storage.
"Under conditions of stable fat mass, one would predict that reduced fat storage would be accompanied by reduced FFA release. We have found that, consistent with this hypothesis, visceral fat is not a major source of fatty acids in the circulation of upper body obese or viscerally obese men and women. In fact, the high FFA levels found in upper body obesity come primarily from upper body subcutaneous fat. We also found that the liver is exposed to some extra FFAs coming from visceral fat in persons with large amounts of visceral fat. Leg fat and upper body subcutaneous fat also have their own unique characteristics that become even more apparent with weight gain."
Some adults develop new fat cells
When normal-weight people gain modest amounts of fat, they do so by enlarging the fat cells in their upper body subcutaneous fat depot. In contrast, gain of lower body fat is largely the result of increasing the number of fat cells. Dr. Jensen highlights: "We found that the gain of as little as 1.2 kg of leg fat resulted in an average gain of 2.6 billion new fat cells! This finding refuted the long-held belief that adult humans do not develop new fat cells but are instead stuck with those that developed in their adolescence. We recently reported that adults do not lose these new leg fat cells when they lose weight.
"New fat cells in adults, like new fat cells in children, come from preadipocytes. Preadipocytes are one of the most common cell types found mixed in among fat cells within adipose tissue. They are typically thought of as capable of replicating and, therefore, of generating a continuous potential supply of preadipocytes and adipocytes. When a preadipocyte receives an appropriate signal from the body, it will cease replicating and develop into a mature adipocyte, which then stores and releases fatty acids under relatively strict hormonal and neural control. Adipocytes also release various hormones, known as adipokines."
Dysfunctional release of fat cells
Dr. Jensen adds: "One of the recent hypotheses regarding why some people become metabolically ill when they become obese and others do not relates to dysfunctional storage and release of fatty acids by adipose tissue. When adipose tissue releases excessive amounts of fatty acids or cannot store them effectively, the fatty acids accumulate in so-called ectopic sites, such as visceral fat, muscle, liver, heart and islet cells. In these tissues, fatty acids can accumulate to excessive amounts in ceramides, diacylglycerols and long-chain acyl coenzyme A's. These fatty acid-containing molecules can serve a signaling function within cells and as such may cause insulin resistance and tissue dysfunction.
"Our laboratory is investigating why some tissues in some people convert fatty acids into abnormal amounts of signaling molecules and others are protected, either by not taking up fatty acids or by storing the fatty acids in the more benign triglyceride form. Understanding these pathways may provide an approach to preventing obesity-related metabolic disorders, such as insulin resistance diabetes, dyslipidemia and hypertension."
From Mayo Clinic Web Site
Subscribe to:
Posts (Atom)